Abstract
BACKGROUND: Patients with Sickle Cell Disease (SCD) have an approximately three-fold higher risk of developing chronic kidney disease (CKD) than the general population. Endothelial dysfunction and inflammation which are induced by hemolysis and lead to vasculopathy are major mechanisms in the development of CKD. Red blood cells (RBCs) hemolysis inside the renal tissue stimulates macrophages infiltration. Endocytosis of RBC hemolysis products by infiltrating macrophages activates to MT-SP1 protease which cleaves and activates non-active circulating Macrophage Stimulating Protein 1 (MSP1). MSP1 binds to and activates cell surface receptor tyrosine kinase, recepteur d'origine nantais (RON).
OBJECTIVES: To determine the role of RON in the development of renal endothelial injury.
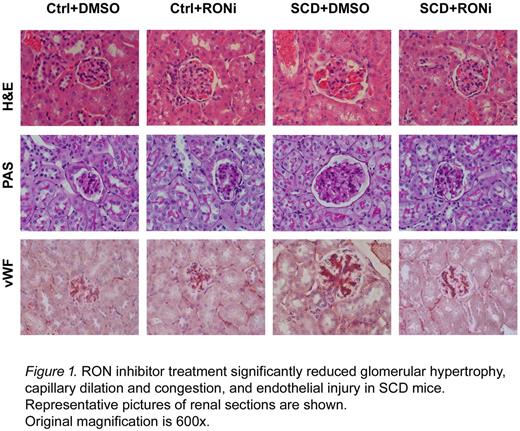
METHODS: Human renal glomerular endothelial cells (HGEC) and a mouse model of SCD (Townes) were used. The animal protocol was approved by the Institutional Animal Care and Use Committee at the Children's National Health System. The SCD mice express human Hgb S and Hgb F. Control mice express human Hgb A1. Two-month-old mice were injected with 10 mg/kg of body weight of RONi (BSM-777607, Santa Cruz Scientific), an inhibitor of RON, subcutaneously daily for 14 consecutive days. Kidneys were collected, and paraffin-embedded sections were used for H&E and PAS staining, and immunostaining.
RESULTS: Treatment of cultured human renal glomerular endothelial cells (HGEC) with MSP1 activated RON receptor and induced downstream signaling evidenced by increased phosphorylation of ERK and AKT kinases. RONi significantly reduced ERK and AKT phosphorylation. MSP1 treatment also increased motility of HGEC, and expression of F-actin and von Willebrand Factor (vWF). Renal disease in SCD mice was characterized by glomerular hypertrophy, capillary dilation and congestion, and significant endothelial injury demonstrated by H&E and PAS staining, and ICAM, vWF and CD34 immunostaining. We observed accumulation of MSP1 in the glomerular capillaries of SCD mice. Treatment of mice with RONi significantly reduced glomerular hypertrophy, capillary dilation and congestion, and also reduced endothelial injury (Figure 1).
CONCLUSIONS: Renal glomerular accumulation of MSP1 and RON kinase activation contribute to the induction of renal endothelial injury in SCD mice. Inhibition of RON kinase activation significantly reduced endothelial injury and development of kidney disease.
ACKNOWLEDGMENTS: This work was supported by NIH Research Grants 1P50HL118006, 1R01HL125005 and 5G12MD007597. The content is solely the responsibility of the authors and does not necessarily represent the official view of NHLBI, NIMHD or NIH.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal